Lupron :: A Primer - Part 1
GnRH analogue hormone commonly known as puberty blocker
Luprorelin :: Generic name
Luprolide Acetate :: US approved name
Lupron :: Brand name marketed + sold by AbbVie
Gonadotropin Releasing Hormone agonist + analogue :: chemical name


Backgrounder on Reproductive Hormones
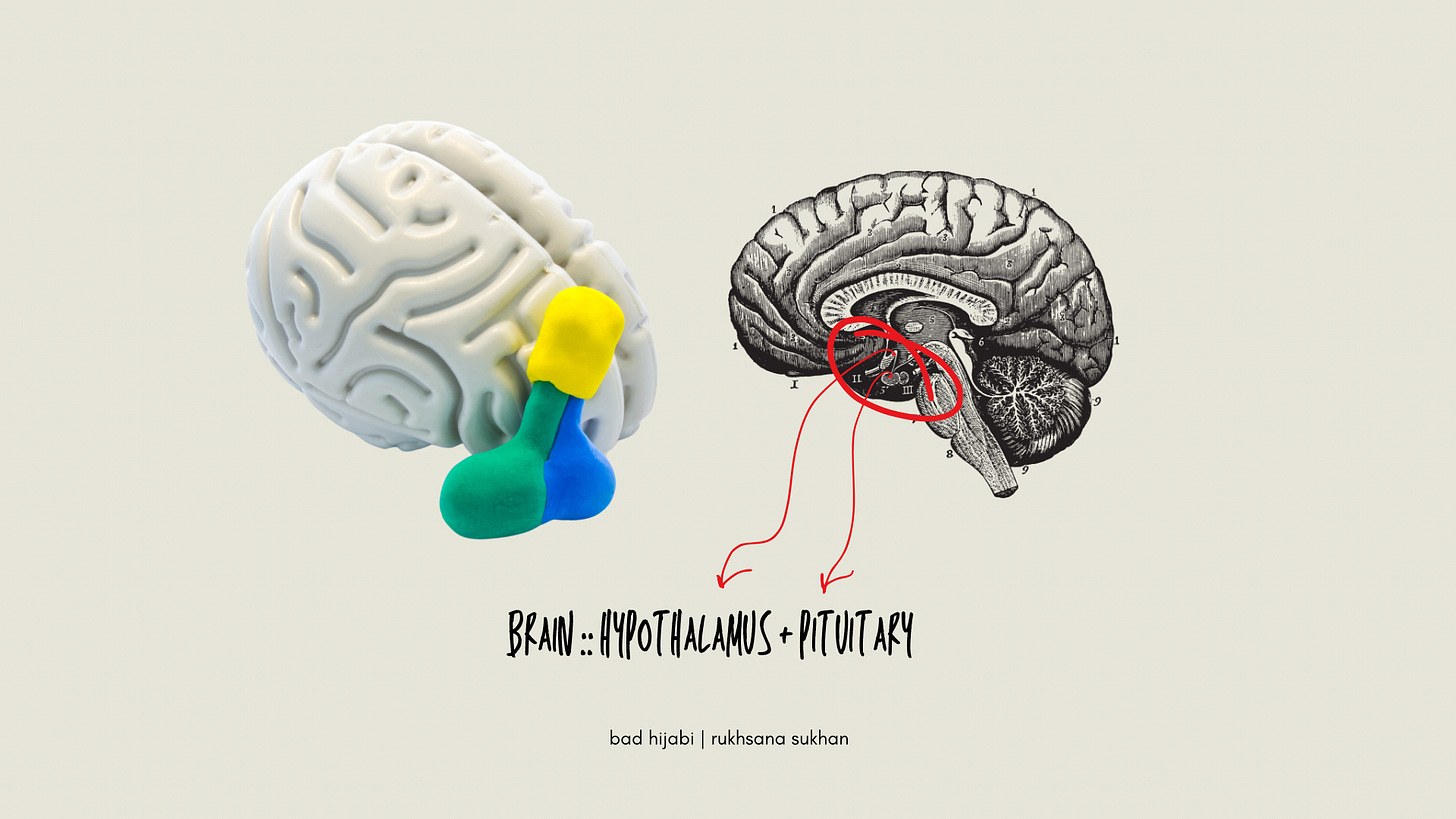
It begins with the hypothalamus, your brain’s control centre, located deep in the centre of the brain, which secrets gonadotropin-releasing hormone (GnRH) in pulsatile fashion.
Then the pituitary, a pea-shaped gland and the master gland of the body that sits just beneath the hypothalamus, wakes up. The pituitary secrets gonadotropins1, more commonly known as leutinising hormone (LH) and follicle stimulating hormone (FSH). Gonadotropins stimulate the gonads to produce sex hormones, estrogen (E) + progesterone (P) and testosterone (T).
In the female reproductive system, FSH stimulates an ovarian follicle to ripen, the level of E rises and an ovum is released. P rises to prepared the uterus for implantation. FSH levels fall and LH levels rise to assist the maturation of the ovum and trigger ovulation and the release of the ovum. This happens around day 14 and it is when the fertile period begins, ie when a woman can get pregnant. The phase governed by LH we call the luteal phase (it is the second half of a 28 day cycle). It involves the build up of the endometrium—this is when uncomfortable premenstrual symptoms occur—and ends with menstruation. Day 1 of the period is the beginning of the cycle—E is low and therefore FSH rises and the cycle repeats.
So, if you want to shut off the reproductive hormone tap, you need to suppress GnRH, which happens in the neurons of the anterior hypothalamus, you can desensitise the pituitary and force it to stop producing gonadotropins.
Backgrounder on Relevant Brain Anatomy
In the image below you can see the hypothalamus + pituitary gland enlarged in the graphic on the LHS graphic and you can see them both to scale on the RHS graphic. This tiny portion of the brain, of which you never think, governs your experiential existence.
Cool, huh?
Fun Fact — Your reproductive system belongs to your neuroendocrine system! Reproductive health vitally impacts the central nervous system and therefore brain health. Descartes was wrong, there is no mind-body dichotomy, the mind is matter we simply cannot see, the mind is a composite of our body’s felt sense in addition to our thoughts which emotions generate — a byproduct of physical and electrical energy fusing inside the human shell case we call the body. Puberty is no more a disease than childbirth or menopause, and it’s important to always remember that we can trigger disease states when we manipulate these three developmental reproductive events irresponsibly.
We exhibit intellectual laziness and dualistic hubris when we presume to conduct clinical science in such as way that divorces reproductive health from neuroendocrine health from psychological health. It truly blows my mind that the present day dominant intellectual ruling class honestly believes that it can manipulate the reproductive axis of human physiology without destabilising neuroendocrine function and without wreaking some kind of enduring unpleasant psychobiological impact!
↪️ The hypothalamus is considered part of the limbic system, a central command post for coping with the challenges of living within our complex social networks.2
↪️ Neurosecretory cells in [preoptic nucleus of ] the hypothalamus … secrete gonadotropin-releasing hormone (GnRH) into blood that travels to the anterior pituitary via the hypothalamo–hypophysial portal system (see image). In the pituitary, GnRH regulates the cells that secrete FSH and LH.3
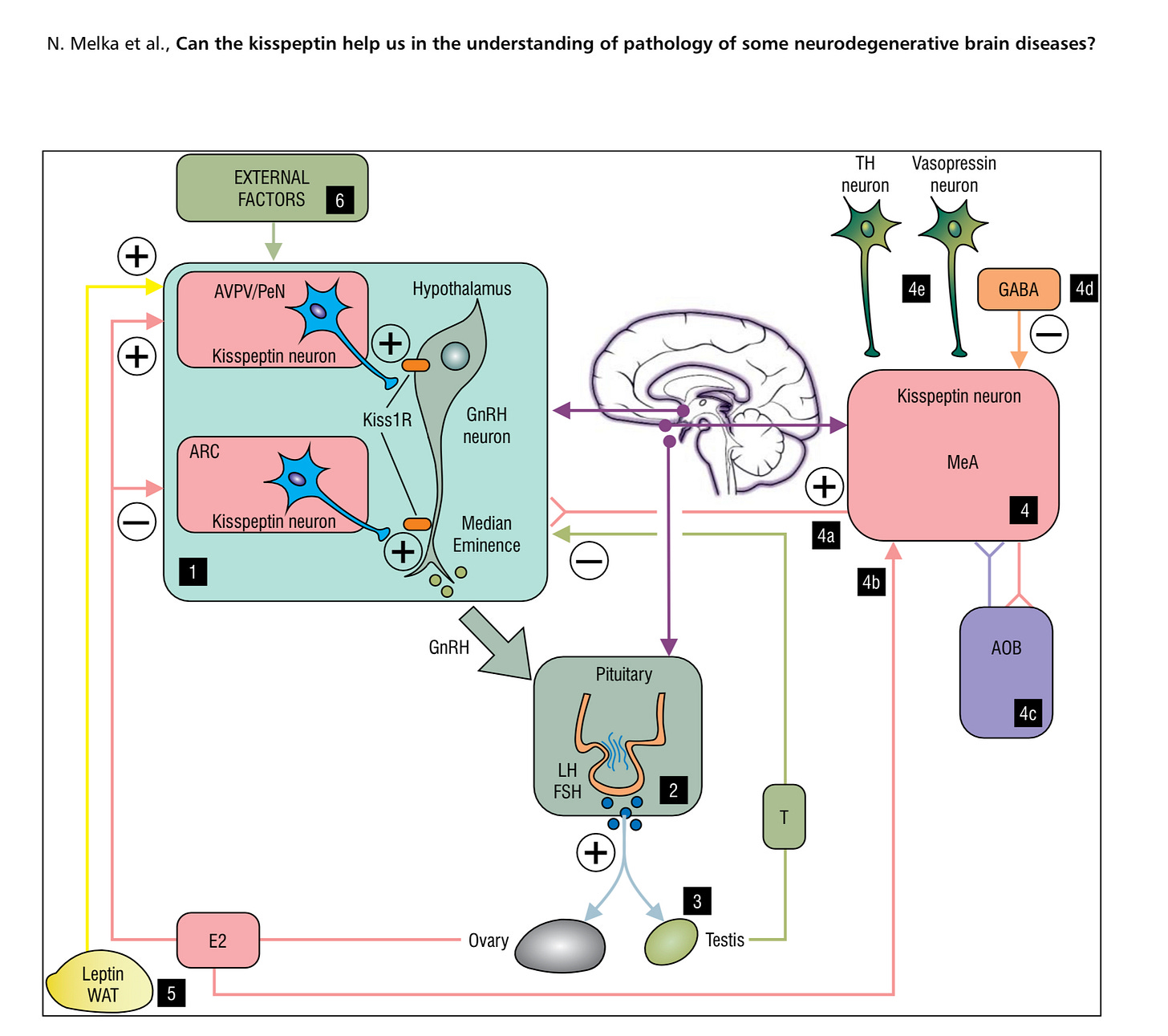
↪️ Kisspeptin is one of the main moderators of the gonadotropic axis … in various regions of the central nervous system … kisspeptin … participates in the regulation of multiple neuronal circuits in the limbic system. The limbic system is a part of the brain involved in behavioural and emotional reactions, and disturbances in its functioning may be the source of some psy- chiatric as well as degenerative disorders.4
↪️ Pituitary desensitization without a feedback loop from the gonads (ie in the case of chemical castration) results in a higher plasma level of FSH (because it has a higher half life than does LH) — FSH levels have an inverse correlation with mood — higher levels of FSH have an association with low mood such as depression + anxiety + irritability.5
The point of this precision-detailed information is to impress upon you, reader, that tinkering with GnRH hormone production + secretion in the body has a more complex and diffuse effect than the mere shutting off of sex.
The hypothalamus is part of the mood + emotion regulation centre of the brain known as the limbic system. Neurons in a particular region of the anterior hypothalamus secrete GnRH to the pituitary gland. A chemical reaction involving a protein called kisspeptin wakes up these neurons so they can secrete GnRH. A feedback loop exists between sex hormone + the kisspeptin mechanism. How does desensitising hypothalamic GnRH neurons impact the kisspeptin neurons? How does suppressing endogenous sex hormone and elevating cross sex hormone impact kisspeptin neurons and the feedback mechanism? How do we account for the impact of circulating gonadotropins (ie FSH) on psychological wellbeing?
Researchers only recently discovered the Kisspeptin protein and its neural signalling mechanism, so we obviously have not considered how gender affirming care modulates kisspeptin signalling and how this will impact children taking Lupron in the long term. There is so much we do not know. There is so much we presume. Why? I like to think of the pubertal intersection of reproductive and neuroendocrine biochemistry as a very complex spaghetti junction in a motorway — tricky to navigate and try to isolate the correct specific path you need to take in order to arrive at your desired destination.
KP plays an important role in limbic system activity, behaviour, and modulation of sex hormones … [and has] antidepressant-like effects. Kisspeptin … activates components of the reward system such as the hippocampus, amygdala and the cingulate and enhances the activity of this system … increases emotional and sexual processing and decreases sexual aversion. Kisspeptin is expressed in the medial nucleus of the amygdala only during puberty.6 The amygdala grows in size and undergoes synaptic pruning as the result of sexual maturation. Kisspeptin has a neuroprotective effect, has positive effects on learning + memory + cognitive functions, and might be implicated in neurgenesis. Decreased kisspeptin signalling decreases brain metabolism. How does a gender affirmation chemotherapy regime of GnRH agonist puberty suppression + cross sex hormone therapy impact functional restructuring of an adolescent brain?7
I find it interesting to read the literature on the clinical research development of Leuprolide Acetate as a treatment and see children with diagnoses of CPP or Endometriosis appear in the literature as a distinct + vulnerable, the language guarded and researchers emphasising caution in using GnRHa on minors. Not all cases of CPP need to be treated, clinicians and families collaborate to make treatment decisions that work in the best interest of the child. Researchers who publish gender dysphoria studies exhibit no such prudence, they exhibit the recklessness characteristic of John Money the psychologist pedophile who experimented on twins, and Harry Benjamin, the sexologist who thought his mission was to change the bodies of those with gender dysphoria to match the way they felt in their minds and who founded the precursor to WPATH.
In nearly 3 decades reproductive science has made leaps and bounds and gender medicine has remained stagnant. We have an ocean of knowledge on one side and then we have a swamp over in the corner. Why?
In 2023 Cohen-Kattenis parrots the same horsehs1t she did in 1996. In 2023, researchers involved in the development of Leuprolide Acetate as a treatment for ovulatory control and for endometrial conditions admitted their naïveté in their initial approaches. The difference between dedicated clinical medical scientist and devoted medical ideologist seems quite staggering to me right now, in the thick of the research, wading through scholarly journal articles and research papers.
Why do we not devote the same level of clinical rigour to young people presenting with symptoms gender dysphoria as we do those with those diagnosed with hypothalamic-pituitary-gonadal axis glandular or gynecological disorders? The obvious answer is dualism — we remain committed to misunderstanding the mind-body connection and to blocking compassionate medicine that prioritises embodied self awareness. The cynical answer is follow the money huny — billionaire ideologue activists who own medical supply companies blah blah blah and their rich oligarch friends are only driving medical activism and political lobby to influence diagnostics + treatment algorithms and not other internal medicine diagnostics + treatment algorithms.
When you work in a field that routinely moves clinical goal posts and redefines diagnostics and concocts baseless treatment regimes in response to political events, and when you are okay with that because you can leverage that for professional gain and narcissistic self interest, then you aren’t a scientist you are a Machiavellian working in science.



The Birth of Leuprolide Acetate
In 1971 Andrew Schally and Roger Guillemin discovered the chemical structure of Gonadotropin-releasing hormone, a molecule comprised of 10 amino acids which “serves as the conductor of the reproductive system and arguably life itself … The elucidation of the amino acid sequence of GnRH was one of the most important events in the field of reproductive medicine.”8 A key finding in the discovery of GnRH involved the activation of GnRH neurons—activation of the reproductive system required a pulsatile stimulation whereas continuous stimulation suppressed the reproductive system. In 1973 Takeda Chemical Industries successfully created a synthetic version of GnRH by altering the endogenous molecular amino acid structure, producing a chemical analogue with a longer half life. In plain speak, this means Takeda created a chemical that looks molecularly similar to endogenous GnRH and has a longer acting time—Leuprolide Acetate has 20 times the potency of endogenous GnRH. This gave scientists the ability to suppress the production of sex hormones from the pituitary gland. This gave scientists the ability to manipulate the Hypothalamic-Pituitary-Gonadal Axis.
Takeda revolutionised the treatment of prostate cancer with the discovery of Leuprolide Acetate because it provided the means for chemical castration, enabling many men to avoid the emotional and psychological effects of surgical castration.
Leuprorelin Acetate had no oral efficacy and in 1985 began patients received their dosage via daily SC or IM injection. The presently established dose, the one-month depot shot, reached market in 1989. At this point Takeda partnered with Abbot to form Takeda-Abbot Partnership (TAP) Holdings to promote Leuprorelin to the American Market. Takeda handled synthesis + manufacturing of the drug and Abbot handled marketing + distribution. TAP Holdings received FDA approval to market + distribute Leuprorelin for the treatment of Prostate Cancer, Endometriosis and Central Precocious Puberty (CPP). TAP received FDA approval for Lupron Depot-Ped in use for CPP in 1993.
Discoveries about the unique pulsatile nature of hypothalamic GnRH-secretion to the pituitary lead to an investigation in the use of Leuprorelin as a fertility agent — as part of IVF protocols that would replace HcG as the first line of ovulation stimulation and therefore dramatically reduce the risk of dangerous side effect of ovarian hyperstimulation sydrome (OHSS). The fascinating complexity of human reproduction and endocrinology can be summed up in the fact that Lupron can function as a chemical castrating agent (in the case of ongoing administration to trigger down-regulation of sex hormones) and also as a fertility agent (in the case of timed administration to trigger a surge). Yet Gender Affirmationists would have you believe in case closed the science is settled. Remember when Lysenko did that to Russian science? Also, do you remember how that went for Russian science?
The Birth of Gender Affirmation Therapy :: Dutch Protocol
Gender Affirming Care originated in the Netherlands in the 1980s and 90s. During his 1993 speech at the Council of Europe Gooren described gender dysphoria (ie the desire to be the opposite sex) as similar to intersex, an sex error of the body, which psychotherapy could not remedy: reassignment of transsexuals is a medical intervention on a sliding scale. It is … a contradiction between the genetic, gonadal and genital sex on the one hand, and the brain sex on the other. Gender Affirming Care emerged from the erroneous belief in mind-body dualism — ie the notion that the brain and the body do not have a connection—which remains a powerful philosophical underpinning of modern psychiatry, despite much evidence to the contrary.
In 1996 Gooren and Delemarre de Waal published their study proposing the use of GnRHa to “delay puberty”, ie “with no permanent effect”, in children with gender dysphoria. It is illegal for a pharmaceutical company to promote any drug for an off-label use. Reading this paper 25 years later seems comical, the researchers truly thought they were delaying puberty and reported their surprise that GnRH agonists did not extend growth time of female-to-male transsexual youth, thereby making them taller than they would have otherwise been.9 The paper also mentions the adrenal suppression + water retention disadvantages of Medroxyprogesterone compared with GnRHa. Gooren and Delemarre de Waal honestly thought blocking GnRH would simply pause the hypothalamus-pituitary-gonadal (HPG) axis with no other effect.
In 1998 Cohen-Kettenis published the second paper promoting GnRHa as a remedy for gender dysphoria. In his 2022 paper Biggs describes the case of FG from CK’s 1998 paper —a lesbian getting a sex change because her father is a homophobe constitutes gay conversion therapy not gender affirming care. Administering GnRHa to minors remained a true exception at this time and Cohen-Kettenis did advocate for lowering the age of administration, in order to bypass puberty altogether and affirm the opposite sex. In 2006 she published a widely read paper, the makers of Triptorelin, an alternative to Lupron, funded the paper.
Gender Dysphoria is an off-label use for GnRHa — Ferring Pharmaceuticals, maker of Triptorelin, promoted an off-label use of it’s product. No FDA on the planet has ever approved any GnRH agonist/analogue in any form ever for treatment of childhood gender dysphoria and that is never in the pipelines because the evidence simply does not exist to get approval. However, Lupron is $424/mo so that provides a great incentive to remain silent whilst clinical activists wage a Gobbelsians campaign to put every kid on puberty blockers.
In his 2022 paper Biggs describes some disturbing failures of the Dutch clinicians to consider minimum age and parental consent for hormone therapy rigourously. As the Cohen-Kettenis puberty blocking protocol began to make headlines worldwide, around the mid-90s, a British documentary called The Wrong Body took three young English people to Amsterdam to see the Dutch gender specialists.
Fred Foley, age 13, met Gooren to learn about puberty suppression … After returning to England and being refused GnHa by the London clinic, Foley's mother telephoned Gooren who agreed to write a three-month prescription of triptorelin. "If your child knows for sure he is transsexual" he said, "I would not let puberty happen.
Some would argue that this example characterises the lack of clinical and diagnostic as well as ethical rigour in gender medicine — very little assessment because of commitment to a particular treatment modality when no evidence exists for that preference. The Dutch Protocol emphasizes two main selling features: 1. fully reversible, and 2. puberty suppression as a diagnostic aide + treatment.
You have to kinda nip puberty in the bud, you want to block it, said Jazz’s mother.
American endocrinologist Norman Spack opened the first gender clinic for kids at the Boston Children’s Hospital in 2007. He established puberty suppression at Tanner Stage 2, which denotes pubertal onset, so age range 8 to 13. Spack set no minimum age, either. Some of the people who oppose this have actually accused doctors of playing God, basically. How do you respond, asked Allison Keyes, 2011 host of Tell Me More. Appealing to a religious text as justification for his zealotry in suppressing child puberty, Spack says the following in this interview with NPR: I go back to the text that guides me in this and that is Leviticus, that says if your neighbor is bleeding by the side of the road, you should not stand idly by.
Spack developed a reputation as a gender affirmation evangelist. To use the evangelical nomenclature of Islam, Spack established his clinic in order to conduct some widespread Gender Identity Dawa10 in children and adolescents. In 2011 Oprah did what she does best and made the pediatric gender movement explode in America, with her feature on Jazz Jennings, then 11 years old. Within a few years the number of pediatric gender clinics exploded, from 1 in 2007 to 40 in 2017.11 SEGM notes there are 60 pediatric gender clinics in the USA and estimates close to 300 clinics and hospitals and medical offices in total deliver puberty suppression to American kids. Spack and his followers truly believe that kids with gender dysphoria, trans kids, have opposite sex brains and therefore justify invasive + experimental hormone and surgical treatments on children to mimic the appearance of opposite sex, which they call gender affirming care.
Maybe the fastest growing religion in American is Gender? The chant of religious fundamentalists then becomes, not Allahu Akbar, but GenderWu Akbar.
Is puberty suppression the confirmation or bat/bar mitzvah of the new Gender religion?
A student of Cohen-Kettenis by the name of De Vries wrote the foundational 2011 + 2014 pediatric gender medicine studies, which catapulted the Dutch puberty suppression Protocol to fame and put child sex change (aka transkids) on the map globally. Despite their designation as gold standard in gender medicine, the De Vries Studies have flaws. First of all subject selection and study design favoured the outcome they wanted — to affirm gender affirming care as an effective treatment for gender dysphoria. Second, the study evaluating the effectiveness of puberty blockers in treating gender dysphoria employed circular logic in evaluating effectiveness. Third the Dutch researchers ignored physical effects (iatrogenic harm) of hormone therapy.
Peggy Cohen-Kettenis wrote about the protocol she developed in 2015, on reading the paper her bias toward gender affirming care for children becomes clear. According to Biggs, Money, who had a reputation for clinical recklessness, praised Cohen-Kettenis in the 80s when she first developed the Dutch Protocol. Having discovered more about the neural origin of puberty, including kisspepin, today we know better—in 2023 Lupron does not seem like the fabulous magical Peter Pan remedy for gender discordant kids that it did in 1996 or 1998 or even 2006.
In January of this year Abbruzzese, Levine + Mason published a critical evaluation of the foundational De Vries Studies. They justify their claims about the flaws in the foundational Dutch research, they discuss the concept of runaway diffusion in the field of pediatric gender medicine, and they offer suggestions for remedying the research weaknesses and flaws in structure. Of particular interest, Abbruzzese et al note that the Dutch researchers applied the UGDS assessment scale in reverse for their post treatment evaluation.
The fact that after gender reassignment, the UGDS scores were low on the opposite-sex scale indicates that the subjects would have scored high on the natal sex scale, which corresponds to a persistence in transgender identity. The finding of persistence of transgender identity is not unexpected, especially since the Dutch researchers selected subjects with lifelong extreme cross-sex identification and follow-up was only 1.5 years post-surgery. What it does not mean is that the feeling of “incongruence” resolved. This point is underscored by the long-term follow-up data on male-to-female Dutch transitioners … Nearly a quarter of the participants have felt that their bodies were still too masculine, and over half have experienced shame for the "operated vagina" and fearful their partner will find out their post-surgical status--despite registering low "gender dysphoria" UGDS scores.
So, to explain in plain language—what the Dutch researchers did to measure the efficacy of their treatment was to have a gender dysphoric female to male patient who at pre-treatment said she felt good when people treated her like a boy score high for dysphoria and then at post treatment the same patient would score low for gender dysphoria still reporting she felt happy when people treated her like a boy. A measurement tool designed to measure the variance between natal sex and gender identity in assessing for treatment cannot then be applied in reverse to determine the efficacy of that treatment. Further, the validation studies for this measurement tool cannot provide the research study which then appeals to the validation study — this is circular reasoning! They could not measure their outcomes? Also, was the goal transforming the child to fit the identity or was it assisting the child to live in his or her body with minimal medical intrusion? The former affirms a construct projected onto a child and the latter affirms the human child.
What is the goal of treatment — to please the clinician or to comfort the patient?
It’s Complicated
I will end this article with this graphic that I have taken from a scholarly paper on the Kisspeptin protein and it’s relationship to GnRH and the HPG axis. The human neuroendocrine system has so many complex moving parts, we really cannot say that we isolate one of these parts during puberty to affirm an adolescent feeling. This is ridiculous, why is anyone taking that claim seriously and offering so many kids up for that experimentation and setting them up with false hopes to attain the unattainable?
I consulted a lot of scholarly references from various areas of scientific and clinical research—because a case of magical thinking and sex denialism has infected the field of gender medicine, and because of the evangelical and activist nature of pediatric gender researchers, the scholarly literature lacks rigour and forces anyone serious about grasping the complexity of puberty and the impact of gender affirming care to wade through many papers on reproductive science, ovulatory control, and the HPG axis.
Leuprolide Acetate celebrates 50 years this years and the American Society of Reproductive Medicine published a special journal issue of papers written by key GnRHa researchers — this proved an invaluable and scientifically rich source of valid and reliable information to reference this article. Puberty is a complex and confounding phenomenon scientists still challenge themselves to fully grasp and so gender affirmationists would do well to restrain their Frankensteinesque arrogance and remember their ethical commitment to DO NO HARM. I also consulted a number of websites, in addition to the drug monographs and historical information. The reference list is extensive and you can find it below the line.
A treatment protocol for adolescents with gender dysphoria: development and evaluation. (2015). Revista Española Endocrinología Pediátrica, 6 Suppl. https://doi.org/10.3266/RevEspEndocrinolPediatr.pre2015.Nov.327
Abbruzzese, E., Levine, S. B., & Mason, J. W. (2023). The Myth of “Reliable Research” in Pediatric Gender Medicine: A critical evaluation of the Dutch Studies—and research that has followed. Journal of Sex & Marital Therapy, 1–27. https://doi.org/10.1080/0092623X.2022.2150346
Biggs, M. (2023). The Dutch Protocol for Juvenile Transsexuals: Origins and Evidence. Journal of Sex & Marital Therapy, 49(4), 348–368. https://doi.org/10.1080/0092623X.2022.2121238
Cohen-Kettenis, P. T., & Van Goozen, S. H. M. (1997). Sex Reassignment of Adolescent Transsexuals: A Follow-up Study. Journal of the American Academy of Child & Adolescent Psychiatry, 36(2), 263–271. https://doi.org/10.1097/00004583-199702000-00017
Cohen-Kettenis, P. T., & Van Goozen, S. H. M. (1998). Pubertal delay as an aid in diagnosis and treatment of a transsexual adolescent. European Child & Adolescent Psychiatry, 7(4), 246–248. https://doi.org/10.1007/s007870050073
De Vries, A. L. C., McGuire, J. K., Steensma, T. D., Wagenaar, E. C. F., Doreleijers, T. A. H., & Cohen-Kettenis, P. T. (2014). Young Adult Psychological Outcome After Puberty Suppression and Gender Reassignment. Pediatrics, 134(4), 696–704. https://doi.org/10.1542/peds.2013-2958
Gooren, L., & Delemarre-van De Waal, H. (1996). The Feasibility of Endocrine Interventions in Juvenile Transsexuals. Journal of Psychology & Human Sexuality, 8(4), 69–74. https://doi.org/10.1300/J056v08n04_05
Littman, L. (2018). Parent reports of adolescents and young adults perceived to show signs of a rapid onset of gender dysphoria. PLOS ONE, 13(8), e0202330. https://doi.org/10.1371/journal.pone.0202330
Littman, L. (2022). Saying that Bauer et al studied rapid onset gender dysphoria is inaccurate and misleading. The Journal of Pediatrics, 245, 250. https://doi.org/10.1016/j.jpeds.2022.03.003
Marchiano, L. (2017). Outbreak: On Transgender Teens and Psychic Epidemics. Psychological Perspectives, 60(3), 345–366. https://doi.org/10.1080/00332925.2017.1350804
Bangalore Krishna, K., Fuqua, J. S., Rogol, A. D., Klein, K. O., Popovic, J., Houk, C. P., Charmandari, E., & Lee, P. A. (2019). Use of Gonadotropin-Releasing Hormone Analogs in Children: Update by an International Consortium. Hormone Research in Paediatrics, 91(6), 357–372. https://doi.org/10.1159/000501336
Chen, T., Yu, W., Xie, X., Ge, H., Fu, Y., Yang, D., Zhou, L., Liu, X., & Yan, Z. (2020). Influence of Gonadotropin Hormone Releasing Hormone Agonists on Interhemispheric Functional Connectivity in Girls With Idiopathic Central Precocious Puberty. Frontiers in Neurology, 11, 17. https://doi.org/10.3389/fneur.2020.00017
Craig, M. C., Fletcher, P. C., Daly, E. M., Rymer, J., Cutter, W. J., Brammer, M., Giampietro, V., Wickham, H., Maki, P. M., & Murphy, D. G. M. (2007a). Gonadotropin hormone releasing hormone agonists alter prefrontal function during verbal encoding in young women. Psychoneuroendocrinology, 32(8–10), 1116–1127. https://doi.org/10.1016/j.psyneuen.2007.09.009
Craig, M. C., Fletcher, P. C., Daly, E. M., Rymer, J., Cutter, W. J., Brammer, M., Giampietro, V., Wickham, H., Maki, P. M., & Murphy, D. G. M. (2007b). Gonadotropin hormone releasing hormone agonists alter prefrontal function during verbal encoding in young women. Psychoneuroendocrinology, 32(8–10), 1116–1127. https://doi.org/10.1016/j.psyneuen.2007.09.009
Friedman, A. J., Juneau-Norcross, M., & Rein, M. S. (1993). Adverse effects of leuprolide acetate depot treatment. Fertility and Sterility, 59(2), 448–450. https://doi.org/10.1016/S0015-0282(16)55701-X
Gooren, L., & Delemarre-van De Waal, H. (1996). The Feasibility of Endocrine Interventions in Juvenile Transsexuals. Journal of Psychology & Human Sexuality, 8(4), 69–74. https://doi.org/10.1300/J056v08n04_05
Influence of Gonadotropin Hormone Releasing Hormone Agonists on Interhemispheric Functional Connectivity in Girls With Idiopathic Central Precocious Puberty. (2020). Front. Neurol, 11(17). https://doi.org/10.3389/fneur.2020.00017
Kuo, C.-Y., Chen, H.-C., & Lee, M.-B. (2014). Leuprolide-Induced Extrapyramidal Symptoms Successfully Treated With Propranolol. Psychosomatics, 55(2), 196–199. https://doi.org/10.1016/j.psym.2013.05.006
LUPRON: MEMORY LOSS AND COGNITIVE. (1996). Lupron Victim Hub. https://www.lupronvictimshub.com/NLVN/NLVNfactsheetMemory.RTF
Melka, N., Pszczolinska, A., Klejbor, I., Ludkiewicz, B., Kowiański, P., & Moryś, J. (2021). Can the kisspeptin help us in the understanding of pathology of some neurodegenerative brain diseases? Folia Morphologica, 80(4), 756–765. https://doi.org/10.5603/FM.a2021.0090
Newton, C., Slota, D., Yuzpe, A. A., & Tummon, I. S. (1996). Memory complaints associated with the use of gonadotropin-releasing hormone agonists: a preliminary study. Fertility and Sterility, 65(6), 1253–1255. https://doi.org/10.1016/S0015-0282(16)58351-4
Rich, S. S., & Ovsiew, F. (1994). Leuprolide acetate for exhibitionism in huntington’s disease. Movement Disorders, 9(3), 353–357. https://doi.org/10.1002/mds.870090317
Rubinow, D. R., & Schmidt, P. J. (2019). Sex differences and the neurobiology of affective disorders. Neuropsychopharmacology: Official Publication of the American College of Neuropsychopharmacology, 44(1), 111–128. https://doi.org/10.1038/s41386-018-0148-z
Sisk, C. L., & Foster, D. L. (2004). The neural basis of puberty and adolescence. Nature Neuroscience, 7(10), 1040–1047. https://doi.org/10.1038/nn1326
Skrapits, K., Sárvári, M., Farkas, I., Göcz, B., Takács, S., Rumpler, É., Váczi, V., Vastagh, C., Rácz, G., Matolcsy, A., Solymosi, N., Póliska, S., Tóth, B., Erdélyi, F., Szabó, G., Culler, M. D., Allet, C., Cotellessa, L., Prévot, V., … Hrabovszky, E. (2021). The cryptic gonadotropin-releasing hormone neuronal system of human basal ganglia. ELife, 10, e67714. https://doi.org/10.7554/eLife.67714
Varney, N. R., Syrop, C., Kubu, C. S., Struchen, M., Hahn, S., & Franzen, K. (1993). Neuropsychologic dysfunction in women following leuprolide acetate induction of hypoestrogenism. Journal of Assisted Reproduction and Genetics, 10(1), 53–57. https://doi.org/10.1007/BF01204441
Wickramasuriya, N., Hawkins, R., Atwood, C., & Butler, T. (2022). The roles of GnRH in the human central nervous system. Hormones and Behavior, 145, 105230. https://doi.org/10.1016/j.yhbeh.2022.105230
Yildirim, M., Mapp, O. M., Janssen, W. G. M., Yin, W., Morrison, J. H., & Gore, A. C. (2008). Postpubertal decrease in hippocampal dendritic spines of female rats. Experimental Neurology, 210(2), 339–348. https://doi.org/10.1016/j.expneurol.2007.11.003
Abbott Company Timeline. (n.d.). [Company Information]. Abbott Company Profile. https://www.zippia.com/abbott-careers-67/history/
AbbVie Win on Humira Patent Portfolio Thwarts Antitrust Attacks. (2022, August 2). Bloomberg Law Review. https://news.bloomberglaw.com/ip-law/abbvie-win-on-humira-patent-portfolio-thwarts-antitrust-attacks
Abouelfadel, Z., & Crawford, E. D. (2008). Leuprorelin depot injection: patient considerations in the management of prostatic cancer. Therapeutics and Clinical Risk Management, 4(2), 513–526. https://doi.org/10.2147/tcrm.s6863
BC Lupron Depot Program for Gender Dysphoria. (n.d.). BC Children’s Hospital. http://www.bcchildrens.ca/endocrinology-diabetes-site/documents/bcchluprongd.pdf
BC PharmaCare Formulary. (n.d.). BC PharmaCare Formulary. https://pharmacareformularysearch.gov.bc.ca/Search.xhtml
Cass Review. (n.d.). Cass Review. https://cass.independent-review.uk/publications/interim-report/
Charatan, F. (2001). Drug companies defrauded Medicare of millions. BMJ (Clinical Research Ed.), 323(7317), 828.
Chwalisz, K. (2023). Clinical development of the GnRH agonist leuprolide acetate depot. F&S Reports, 4(2), 33–39. https://doi.org/10.1016/j.xfre.2022.11.011
Closure of Britain’s Tavistock clinic rekindles heated debate on trans youth. (2023, March 25). Le Monde. https://www.lemonde.fr/en/m-le-mag/article/2023/03/25/closure-of-britain-s-tavistock-clinic-rekindles-heated-debate-on-trans-youth_6020598_117.html
Column: A transgender patient’s lawsuit against Kaiser is a front for the conservative war on LGBTQ rights. (2023, March 3). LA Times. https://www.latimes.com/business/story/2023-03-02/transgender-patients-chloe-cole-lawsuit-against-kaiser-lgbtq-rights
Eguale, T., Buckeridge, D. L., Verma, A., Winslade, N. E., Benedetti, A., Hanley, J. A., & Tamblyn, R. (2016). Association of Off-label Drug Use and Adverse Drug Events in an Adult Population. JAMA Internal Medicine, 176(1), 55. https://doi.org/10.1001/jamainternmed.2015.6058
Food and Drugs Act (R.S.C., 1985, c. F-27). (n.d.). Food and Drugs Act (R.S.C., 1985, c. F-27). https://laws-lois.justice.gc.ca/eng/acts/f-27/page-2.html#h-234115
Fujino, M., Fukuda, T., Shinagawa, S., Kobayashi, S., Yamazaki, I., Nakayama, R., Seely, J. H., White, W. F., & Rippel, R. H. (1974). Synthetic analogs of luteinizing hormone releasing hormone (LH-RH) substituted in position 6 and 10. Biochemical and Biophysical Research Communications, 60(1), 406–413. https://doi.org/10.1016/0006-291X(74)90219-8
Guidance Document - Health Canada and Advertising Preclearance Agencies’ Roles Related to Health Product Advertising. (2010). Health Canada. https://www.canada.ca/en/health-canada/services/drugs-health-products/regulatory-requirements-advertising/policies-guidance-documents/advertising-preclearance-agencies-health-product.html
How a Drug Company Made $114 Billion by Gaming the U.S. Patent System. (2023, January 28). New York Times. https://www.nytimes.com/2023/01/28/business/humira-abbvie-monopoly.html
Humaidan, P., & Haahr, T. (2023). GnRHa trigger—the story of the ugly duckling. F&S Reports, 4(2), 15–19. https://doi.org/10.1016/j.xfre.2023.02.011
Humira Shows That America’s Patent Innovation System Is Working. (2023, February 23). Bloomberg Law. https://news.bloomberglaw.com/us-law-week/humira-shows-that-americas-patent-innovation-system-is-working
Institute for Research On Public Policy: Policy Options. (n.d.). Institute for Research On Public Policy: Policy Options. https://policyoptions.irpp.org/magazines/from-climate-change-to-clean-energy/reimbursing-a-drug-off-label-its-what-you-dont-know/
Journalist Hannah Barnes on the inside story of the collapse of Tavistock’s gender identity clinic. (2023, March 9). WBUR On Point. https://www.wbur.org/onpoint/2023/03/09/the-inside-story-of-the-collapse-of-the-tavistock-gender-service-for-children
Kim, J. Y., Lee, J. H., Cho, H.-H., & Kim, H. S. (2020). Incidental Findings on Brain Magnetic Resonance Imaging in Children with Central Precocious Puberty. The Ewha Medical Journal, 43(4), 53–59. https://doi.org/10.12771/emj.2020.43.4.53
Lambalk, C. B. (2023). The enigma of the gonadotropin-releasing hormone pulse frequency governing individual secretion of luteinizing hormone and follicle-stimulating hormone. F&S Reports, 4(2), 27–32. https://doi.org/10.1016/j.xfre.2023.02.010
Lee, C. C., Najafzadeh, M., Kesselheim, A. S., & Sarpatwari, A. (2021). Cost to Medicare of Delayed Adalimumab Biosimilar Availability. Clinical Pharmacology & Therapeutics, 110(4), 1050–1056. https://doi.org/10.1002/cpt.2322
Lupron Drug Monograph — AbbVie. (n.d.). AbbVie Canada. https://www.abbvie.ca/content/dam/abbvie-dotcom/ca/en/documents/products/LUPRON_CPP_PI_EN.pdf
Medical Affirmation and Transition. (n.d.). Trans Care BC. http://www.phsa.ca/transcarebc/child-youth/affirmation-transition/medical-affirmation-transition#Puberty--blockers--and--hormones
Paulson, R. J., & Gordon, K. (2023). Gonadotropin-releasing hormone: incredible 50 years. F&S Reports, 4(2), 1–2. https://doi.org/10.1016/j.xfre.2023.03.007
Plan G Psychiatry Meds. (n.d.). BC Health. https://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/pharmacare/pharmacare-publications/pharmacare-policy-manual-2012/coverage-plans/psychiatric-medications-plang
Prescription Pharmaceuticals in Canada: Off Label Use. (2014). Canadian Senate Standing Senate Committee on Social Affairs, Science and Technology. https://sencanada.ca/content/sen/Committee/412/soci/rep/rep05jan14-e.pdf
Reckless and Irresponsible The ACLU pushes the potent but misleading “affirm or suicide” narrative. (2023, March 17). City Journal. https://www.city-journal.org/article/reckless-and-irresponsible/
Rubinow, D. R., & Schmidt, P. J. (2019). Sex differences and the neurobiology of affective disorders. Neuropsychopharmacology, 44(1), 111–128. https://doi.org/10.1038/s41386-018-0148-z
Schally, A. V., Arimura, A., Baba, Y., Nair, R. M. G., Matsuo, H., Redding, T. W., Debeljuk, L., & White, W. F. (1971). Isolation and properties of the FSH and LH-releasing hormone. Biochemical and Biophysical Research Communications, 43(2), 393–399. https://doi.org/10.1016/0006-291X(71)90766-2
Sharafuddin, M. J., Luisiri, A., Garibaldi, L. R., Fulk, D. L., Klein, J. B., Gillespie, K. N., & Graviss, E. R. (1994). MR imaging diagnosis of central precocious puberty: importance of changes in the shape and size of the pituitary gland. American Journal of Roentgenology, 162(5), 1167–1173. https://doi.org/10.2214/ajr.162.5.8166005
UK woman who regrets teen gender transition sees court victory overturned on appeal. (2021, September 17). Catholic News Agency. https://www.catholicnewsagency.com/news/249026/keira-bell-uk-woman-who-regrets-teen-gender-transition-sees-court-victory-overturned-on-appeal
Walters, K., Wegorzewska, I. N., Chin, Y.-P., Parikh, M. G., & Wu, T. J. (2008). Luteinizing Hormone-Releasing Hormone I (LHRH-I) and Its Metabolite in Peripheral Tissues. Experimental Biology and Medicine, 233(2), 123–130. https://doi.org/10.3181/0707-MR-201
Will Humira Biosimilars Entry Cause a Wave or a Ripple? (n.d.). Pharmacy Practice News. https://www.pharmacypracticenews.com/Policy/Article/05-23/Will-Humira-Biosimilars-Entry-Cause-a-Wave-or-a-Ripple/70262
Yildirim, M., Mapp, O. M., Janssen, W. G. M., Yin, W., Morrison, J. H., & Gore, A. C. (2008). Postpubertal decrease in hippocampal dendritic spines of female rats. Experimental Neurology, 210(2), 339–348. https://doi.org/10.1016/j.expneurol.2007.11.003
gonadotropin = gonad (reproductive organs, either ovaries or testes, which secrete sex hormones ) + tropin (stimulating the effect of on a target organ) = hormones that stimulate the gonads to produce sex hormones.
van Der Kolk 2014, p. 56
Melka et al, 2021
Melka et al, 2021
Paulson + Gordon, March 2023
Dawa = conveying the message to non-believers


