Eby Government Won’t Renew Contracts with US Clinics for BC Cancer Treatments
apparently it’s unrelated to the the government’s policy to eliminate contracting to US companies wherever possible
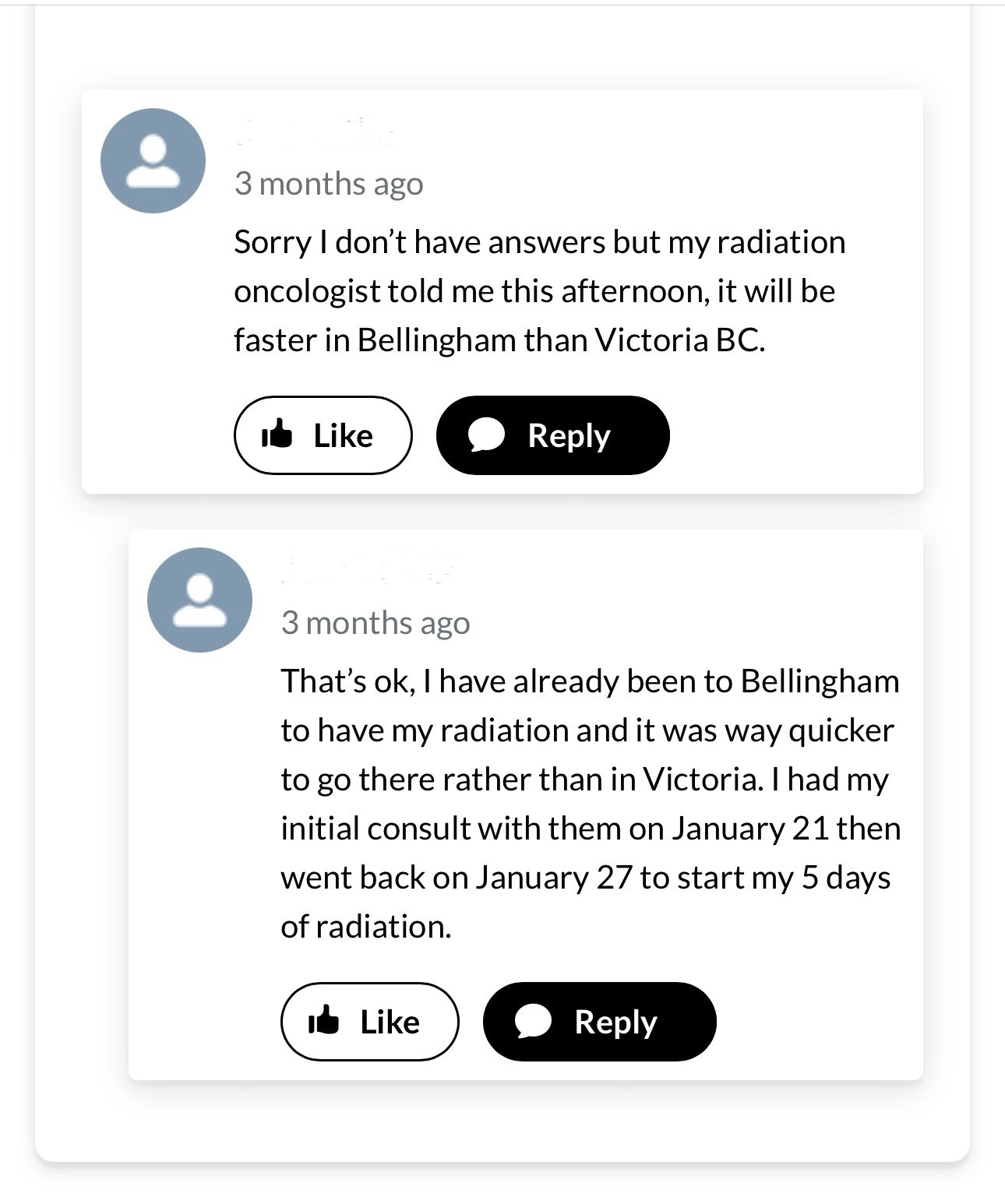
Nearly three months ago the Eby government committed to the continuation of cancer treatment in Bellingham. A month ago the Eby government announced it would not renew the contracts with the two Bellingham clinics operating under PeaceHealth. The contracts with PeaceHealth to provide radiation treatment at St. Joseph Cancer Center and North Cascade Cancer Center expire at the end of May. Despite the ongoing crisis of care taking place in the BC patient care system, the Eby government insists that it will not compromise care by ending the supposed temporary programme which referred cancer patients to the Bellingham cancer centres to receive timely radiation treatment.
British Columbians still report lengthy wait times for treatment and even to see an oncologist. Rural communities suffer the most from the inadequate health care system — facing ER closures, and a lack of oncology and other specialist clinics, and facing lengthy waits times for everything, and on top of that facing the prospect of travelling to receive health care. The Eby government’s April 7th news release says that, as of the end of February 2025, approximately 93% of patients in B.C. were waiting less than four weeks to start their radiation treatment – exceeding the national benchmark of 90%. This is also a 24% improvement since spring 2023, when only 69% of patients were starting treatment within four weeks. On April 10th, Eby announced his intention to eliminate contracts with American companies wherever possible. It’s unknown whether the decision not to renew the contract is related to that new policy.
“The primary factor in all of this is the lack of healthcare professionals and infrastructure needed. Our focus is ensuring that further inequity doesn't occur [because of] your address.” — Paul Adams, Executive Director, BC Rural Health Network, 24.4.2025
Reader, I would think the statistics would signal the programme works to relieve the strain and serve patients in a more timely and efficacious manner. I would think the statistics would encourage the government to continue, and not only try to reach that capacity of 50 patients per week, but also in tandem with reducing wait times in rural areas even further whilst optimising patient access to ensure program capacity. I would think this would take place whilst we ensure we build up the system’s capacity, so that one day we truly do not need to go to an America cancer centre to receive radiation therapy. Reader, I wouldn’t take these statistics as a signal to end the program, ie to decide we don’t need to renew the contract with PeaceHealth.
Reader, WTF is all I can say. It seems foolish and hasty. We have not built up sufficient capacity to eliminate that PeaceHealth radiation treatment program. I wonder out loud how much TDS drives this policy decision. If that’s the case it would be reckless and foolish. It says Ideas > Humans and that’s evil.
Whilst I and others can sit here and write about wait times in the BC healthcare system, and whilst the Eby government can say, look we exceed the national benchmark for wait times, we’re good, and whilst BC Health Coalition and other anti-privatisation activists can maybe say, hey that’s good we shouldn’t be outsourcing health care anyway blah blah public healthcare blah blah, America is bad blah blah, the fact remains waiting sucks when you’re sick and waiting for a specialist or treatment or for reconstructive surgery, plunged in choicelessness and uncertainty. The fact also remains that travelling far from home to receive healthcare treatment costs in human and financial terms and we cannot make that a long term solution. Delivery of health care should be the same, no matter where you live in the province — that’s what universal access means.
Health care goes well beyond numbers like wait times and fiscal thresholds and other beancounter details. Healthcare means humans, it means sick humans need care to get well. Patients face uncertainty, fear, choicelessness in addition to their body malfunctioning. Being sick sucks, holistically, it bloody sucks. The fact remains sick people will choose the option that gives them the most timely treatment for the best quality of live and survival. People will choose a thing that gives the a semblance of certainty. People want to feel in control, choices give them that control.
Whether or not it’s politically correct to continue relying on outsourcing treatment to America cancer clinics, whether or not healthy activists feel okay with privatisation and outsourcing to American healthcare providers, well that seems besides the point.
Humans > Ideas.
Here’s a very heartbreaking story from an online cancer support group about waiting for reconstructive breast surgery.
Let me paint the scene: I’m currently awaiting surgery number five. Yes, five. This one is the big one—the DIEP flap reconstruction. You know, the surgery that’s supposed to make me feel whole again. Like a woman with breasts who doesn’t have to stuff her bra like a teenager at a middle school dance.
I've technically been waiting since 2022. But life, in all its unpredictable chaos, had other plans … By the time I got the green light for surgery in September 2024, I was running on fumes—but hopeful. Finally, I thought. Finally. I was booked for January 2025.
Spoiler alert: canceled.
But it’s okay, they said. You’re rescheduled for February. Just a short hop away.
Canceled.
Okay... March? Nope. April? Nope. May? Big fat nope. Apparently, no really is a full sentence … I know there are newly diagnosed women who urgently need those OR spots. And I swear—I do understand. But understanding doesn’t make it less gutting when you’ve been emotionally prepping for a surgery that keeps getting ripped out from under you like a bad magic trick.
When will it be my turn? When do I get to lie naked on that cold operating table and be sewn back together into something that resembles the me I used to know?
I hate that I’m angry. I hate how powerless this makes me feel. But that’s what waiting does—it wears down your bones and frays your nerves. It messes with your mind, body, and soul. It teaches you humility, sure, but also desperation. And let’s be real: I’m out here trying to heal, not audition for the next season of Survivor: Surgical Standby Edition.
Reader, how can we kid ourselves about our supposedly fabulous national healthcare system, how can we keep bragging about how no one has to go bankrupt to receive treatment, how it’s free healthcare blah blah, when people battling the system for care feel broken by a broken system? One response to this heartbreaking description of waiting for surgery summarises well the dilemma, many of us can relate to your post, as the waiting game is so hard. Our medical system is so broken.
How can anyone who’s desperately trying to move on with life and heal, following a battle with cancer, do so when the system kicks them down, repeatedly? Reader, go back and reread that quote: waiting … wears down your bones and frays your nerves. It messes with your mind, body, and soul … it teaches you … desperation.
A recent report by BC Rural Health has found that people feel frustrated because the government doesn’t listen to them and engage with them to meet their healthcare needs. I will write more about this in a future article. A recent story appeared in Interior News, reporting that the emergency department at Lakes District Hospital and Health Centre has closed for the 20th time in 2025. According to the story, written by Jake Wray, who spoke with officials at Northern Health, “Burns Lake is currently experiencing an approximately fifty-five per cent vacancy rate for physician emergency room coverage.”
Paul Adams, executive director of the B.C. Rural Health Network, says he is cautious about what the cancellation of this program could mean for the wait list of people awaiting treatment, particularly when work to add regional cancer care centres across the province is not complete, reports CBC news. Adams has previously expressed his concern about BC cancer patients having to rely on receiving treatment from the US, and he reiterated that concern in email correspondence with me today. Reader, rightly so, Canadians having to rely on their provincial health authorities to outsource their healthcare treatments to American clinics doesn’t serve them over the long term. We pay taxes for Canadian health care, so the thought of travelling across the 49th parallel to receive Canadian taxpayer funded healthcare seems dystopian. Nonetheless, patients require access to healthcare treatment in a timely fashion and they will go where they can receive that.
What’s the answer, reader? I don’t know.
I only know that it’s a form of torment, being forced to wait for cancer treatment when you’re sick and trying to heal and move on with life. I only know that it’s also torment to have to wait 3 years for reconstructive breast surgery, after battling breast cancer for 6 years. Reader, how can we brag about our health care system when it’s failing the most vulnerable so miserably? In our email, Paul Adams told me what most of us know.
“The system needs to change. We need to have team based care supports and attachments to a place of care rather than an individual, we are keen supporters of true Community Health Care models that create these environments (and especially in rural communities). We also need to change a system from one of convenience to the administrative side to one of service to the client. An example of the inefficiencies in the system is the lack of personalized service provision from an overburdened system. People are not recognized within the system as individuals but as a requisition [number] that needs to be processed.” — Paul Adams
Can the Eby government guarantee that wait times for radiation treatment will meet the standard the PeaceHealth radiation program has provided those who opted to go to Bellingham for their treatment? Do we really believe that choosing not to renew that contract in the interest of public healthcare will best serve the sick and ailing who wait and wait and often get told to keep waiting? Have we done enough to build up capacity in the system? When it comes to healthcare delivery, centralised does not equal universal.
“BC has failed to build out capacity in healthcare for 30+ years but investments that are being made now (although late) are absolutely necessary and will provide the level of care needed once complete. As you stated this takes time. In many ways we have two tier systems now that are complex and not entirely public. We remain committed to supporting universal public healthcare systems that fulfill the requirements of the Canada Health Act and specifically section 12.1.a.
If private delivery is an aspect of that system (which it is) this must not equate to user pay for access. Reasonable access must be provided without financial or other barriers as per section 12 .1.a. the CHA to all insured residents. That is the insurance policy we have and should require our governments to uphold. Times have changed and much more needs to be done to ensure that a strong and robust universal healthcare system is in place for the future. Much of the work requires a change in approach and a change in how we view costs to the system. To minimize the cost to everyone the best mythology is to create health and wellness in the population, this will drastically and naturally reduce costs in the future but requires immediate investment up front and both politics and short-term budgeting create many challenges.” — Paul Adams
The Eby government says it’s exceeded national benchmarks for treatment wait times so it can feel confidently about stopping the radiation treatments in Bellingham. When I asked Paul Adams his thoughts on this he told me welcomed the reduced wait times and noted that a system which centres administration and not people serves patients poorly.
“We see the reduced wait time as a positive and many choices are not in the hands of patients generally and we are subjected to the system as it is. For patients with their own resources and ability to fund their healthcare directly they still have a choice to seek treatment anywhere they choose. We have not built out our system to the degree needed in many ways, but we have built out capacity more in the last 5 years than we have in decades and this is both welcome and needed. Many people are impacted by many gaps in services and we need to do much more and as you stated this all takes time. Is sending people out of country for treatment a practical long-term solution, probably not.” — Paul Adams
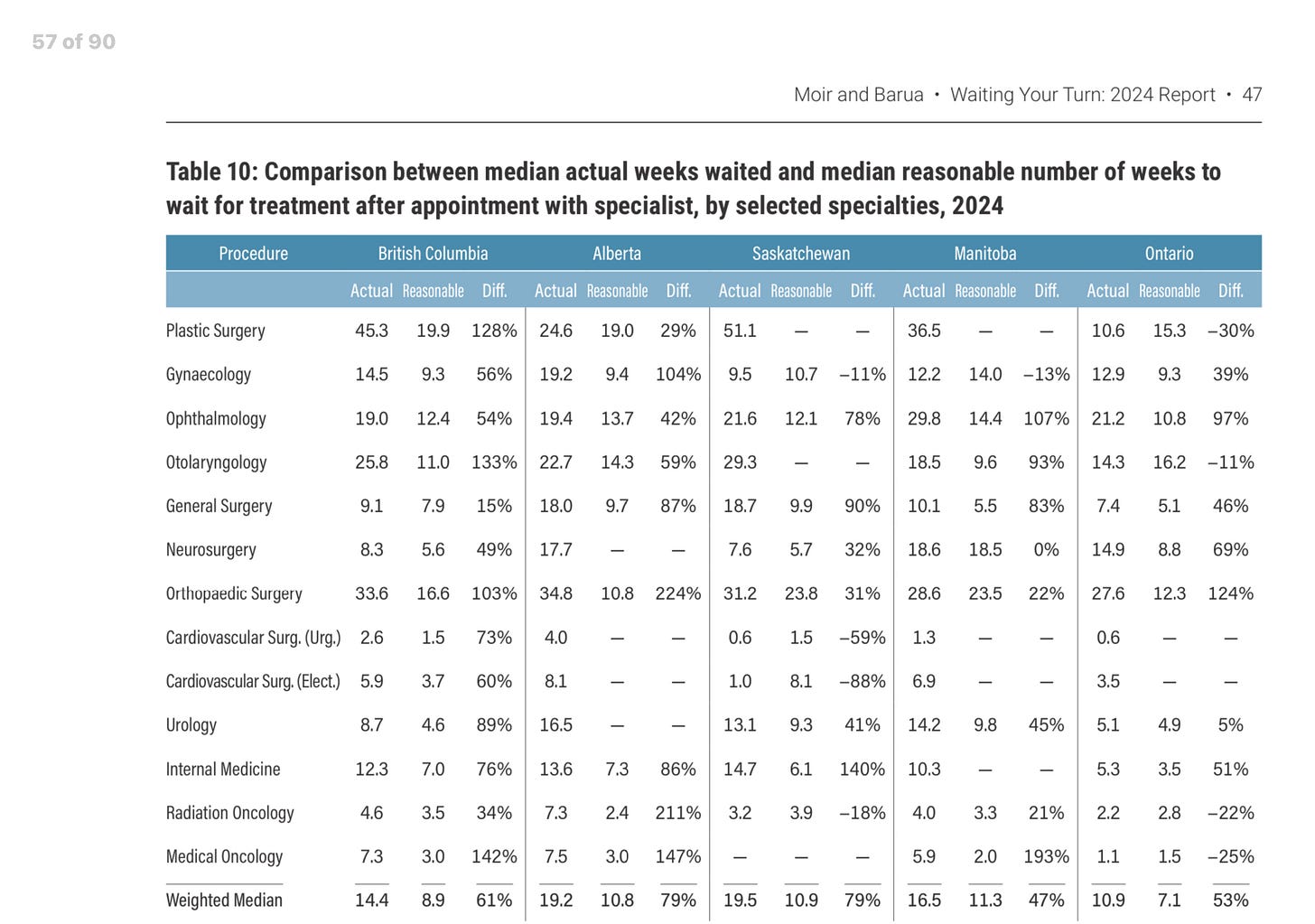
A recent report by the Fraser Institute on wait times for healthcare treatment procedures in Canada shows that BC has amongst the highest wait times from GP to specialist to treatment delivery in the country. Waiting Your Turn tells the statistical tale of how nearly 4% of Canadians across the country are waiting for medically necessary healthcare treatment. Waiting Your Turn reports the longest wait time in the history of the annual survey.
Whilst the PeaceHealth radiation treatment program occupies a narrow band of healthcare treatment, it’s poor optics for a government to remove an option that improves access to cancer treatment at a time when the system as a whole remains very broken and on the brink of collapse. It means taking options away from people who’ve already suffered an involuntary plunge into forced choicelessness because of illness and related hardships. Psychologically, this impacts healthcare, because neurological and endocrine, and cardiac and respiratory and haematological and renal and hepatic and bowel health all depend on emotional and psychological factors. Waiting whilst plagued by fear and uncertainty makes people feel sicker. It breeds desperation.
Reader, this is not socially just. It is not progressive. It is not inclusive. It is not diverse. It is not compassionate. Reader, it is unnecessary. The government established the program for a reason, to meet unmet needs. The program added capacity and it seemed to reduce wait times. It gave people a choice in a system where not enough choices exist for those who desperately need them. However, as Paul Adams told me, it’s unreasonable to expect to send patients to the USA to receive health care over the long term — we need made in Canada solutions for Canadians, we need patient-centred care, this means a profound shift in the way we administer and organise and plan care. We need to work more diligently at building capacity in our healthcare system, it’s a complex problem which demands a complex multifocal solution.
“BC is not like any other place in Canada or in the world, our geography, low population density and climate all make BC unique and for us we need better made in BC solutions that we believe exist but need to be invested in now for tomorrow. We need to plan for future generations and not for who the next government will or won't be. Politics don't work well in healthcare planning.” — Paul Adams, 24.4.2025
This article is part of a series I’ve decided to write about health care in British Columbia. I had an in-depth email conversation with Paul Adams, he raised some important points and I plan to write several more articles about the health care system in BC, specifically how it’s failing British Columbia’s and what’s needed to fix our broken system.






It’s not just BC. Our Soviet-style healthcare system is broken everywhere, yet all of our politicians insist it can never be changed. The only other country in the world that emulates the Canadian system is North Korea. All the others- and especially the ones that have shorter wait times than us - have some mix of public and private providers.